Background: Daratumumab is an anti-CD38 monoclonal antibody approved in combination with pomalidomide/dexamethasone (DPd) and carfilzomib/dexamethasone (DKd) for patients with relapsed/refractory multiple myeloma (RRMM). We conducted a large multicenter retrospective study to analyze the safety and efficacy of DPd versus (vs) DKd in daratumumab naïve RRMM patients treated in real-world practice.
Methods: We evaluated RRMM patients who had received either DPd or DKd for RRMM at the University of Kansas Cancer Center and Medical University of South Carolina between January 2015 and June 2022. Daratumumab was given as daratumumab 16 mg/kg IV or 1800 mg SQ weekly for cycles 1 and 2, every 2 weeks for cycles 3-6, and then every 4 weeks in both groups. In the DPd group; pomalidomide (pom) was dosed at 4 mg orally on days 1-21 of a 28-day cycle, and dexamethasone 20 mg (age>75) or 40 mg (age≤75) weekly. In the DKd group; IV carfilzomib was given at 70 mg/m 2 day 1, 8, 15 every 4 weeks; dexamethasone 20 mg (age>75) or 40 mg (age≤75) weekly. Doses and frequency of chemotherapy were adjusted for toxicities per the package insert and physician discretion. Responses were evaluated using IMWG criteria and toxicities were graded using common terminology criteria for adverse events (CTCAE). Patient and disease characteristics, as well as safety and efficacy outcomes were summarized with descriptive statistics. Kaplan-Meier analyses were used to estimate progression-free (PFS) and overall survival (OS).
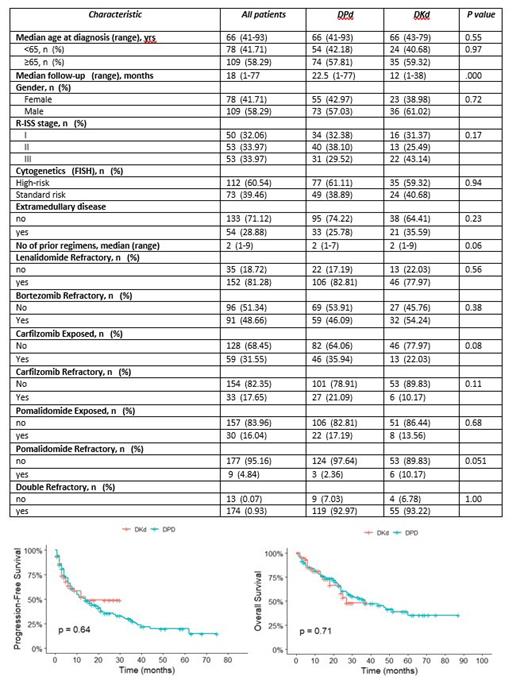
Results: A total of 187 pts with RRMM were included in the analysis; 128 patients received DPd, and 59 pts received DKd. The median age for the entire patient population was 66 years (range 41-93), 109 (58.29%) patients were male, 110 (59.46%) had IgG isotype, 53 (33.97%) had R-ISS stage III disease, 112 (60.54%) had high-risk cytogenetics (del 17p, t(4;14), t(14;16), gain or amp 1q), and 54 (28.88%) patients had extramedullary disease (EMD) (Table 1). Patient and disease related characteristics in two groups appeared equally balanced except for numerically more patients in the DKd group with RISS III, EMD, and pom refractoriness. A vast majority of patients had lenalidomide refractory disease (~80% in each group) and nearly 50% had bortezomib refractory disease in each group. A total of 32 (54.24%) patients who had bortezomib refractory disease received DKd while only 3 (2.3%) patients with pom refractory disease received DPd.
The overall response and very good partial response rates were 80.46% and 14.06% in the DPd group vs 79.65% and 11.76% in the DKd group, respectively. With a median follow up of 18 (1-77) months for the entire patient population, median PFS was 14 months (9-21) and 14 months (7-not reached (NR)) (p=0.64) for the DPd and DKd groups, respectively (Figure 1). Similarly, median OS was 37 months (27-NR) and 27 months (24-NR) (p=0.71) for DPd and DKd groups, respectively (Figure 1). The most common grade 3+ adverse events were neutropenia (32.02% vs 6.77%), anemia (14.05% vs 10.17%), thrombocytopenia (12.48% vs 15.24%), and cardiovascular events (3.91% vs 15.25%) in the DPd vs DKd groups, respectively. Serious adverse events requiring hospitalization occurred in 43.7% in the DPd group vs 33.9% in the DKd group. More patients in the DPd group required dose reductions (53.12% vs 18.63%) or dose delays (48.4% vs 30.51%) due to toxicities (cytoepenias) than the DKd group. None of the patients required permanent discontinuation related to adverse events.
Conclusion: This is the first and largest reported study of DPd vs DKd for daratumumab naïve patients in a real-world setting. Both DPd and DKd appeared to be a safe and effective treatment options for RRMM. While there were more cytopenias associated with DPd and more cardiovascular side effects with DKd, there were no significant differences in the depth and duration of remission with these two regimens. Prior exposure, drug-class refractoriness, high risk disease features, and patient comorbidities need to be taken into consideration for the choice of therapy for RRMM.
Disclosures
Ahmed:BMS: Consultancy; Kite: Consultancy, Research Funding. Hashmi:Karyopharm: Speakers Bureau; BMS: Honoraria; Jannsen: Honoraria, Speakers Bureau; Sanofi: Honoraria, Speakers Bureau; GSK: Honoraria, Speakers Bureau.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal